Who are Paediatric Psychosocial Service
The Paediatric Psychosocial Service (PPS) is a specialist CAMHS team (Child and Adolescent Mental Health Service) for children and young people who are being treated at the Royal Manchester Children’s Hospital. We provide psychological and psychiatric assessment and treatment for patients who face emotional and mental health challenges related to their underlying physical illness.
We’re a diverse and inclusive team, made up of people with a wide range of backgrounds, experiences, and identities, and we’re committed to fostering a culture that values and celebrates that diversity.
Our Team Includes:
- Consultant Clinical Psychologist and Strategic Lead for Paediatric Liaison
Sarah Gaskell - Consultant Psychologists
Dr. Stewart Rust
Dr. Louise Robinson
Dr. Claire Brown
Dr. Ruth Hurrell
Dr. Paul Abeles - Consultants Psychiatrists
Dr. Neelo Aslam
Dr. Shruti Garg
Dr. Hema Ramalingam - Assistant Operational Manager
Lilian Sanchez - Office Manager
Katie Kelly
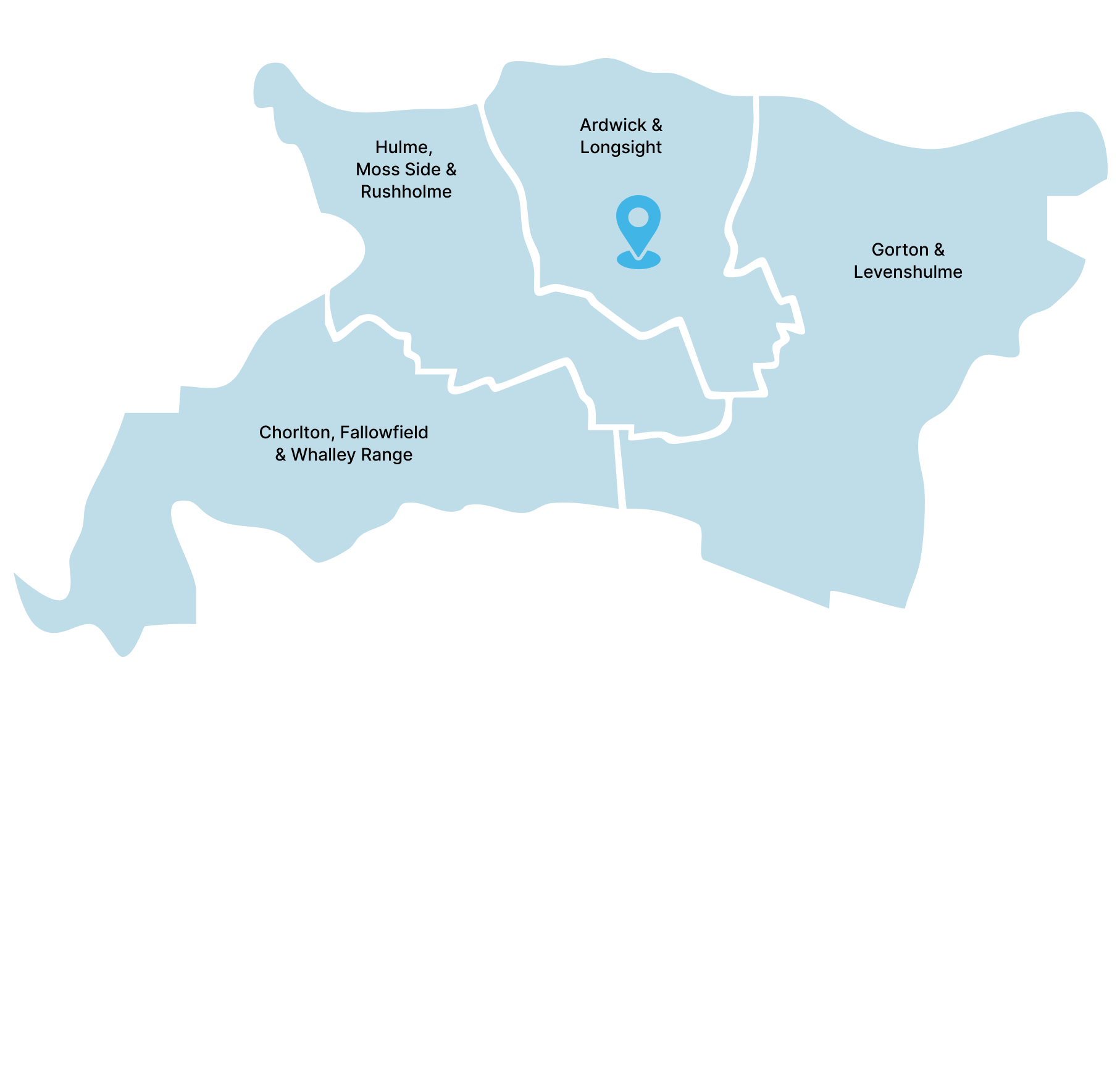
Paediatric Psychosocial Service Location
Address:
Harrington Building, Hathersage Road, Manchester, M13 9WL (Opposite Peter Mount Building) Car Park: Hathersage Road car park. You make payment on exiting the car park, the usual charge is £2.50 for up to 3 hours.
View MapContact Details:
In need of urgent help?
Get Urgent Help NowAccess to PPS
Coping with complex health problems can be difficult for everyone at times, and there may be problems that we can help with.
A member of your medical team may ask you if you would like to be referred or you can also speak to them if you would like to access our Service. Medical teams can refer to us via HIVE (the MFT electronic patient care record) or by email to the address above.
A wide range of specialist assessments and interventions are offered. These include:
- Neuropsychological and cognitive assessments
- Cognitive-behavioural approaches
- ACT (Acceptance and Commitment Therapy)
- EMDR
- CFT Compassion-Focused Therapy)
- Solution-focused
- Systemic
- Narrative
- Family Therapy
- Neuropsychological rehabilitation
- Group work
(e.g. Tree of Life; Chronic Pain – Pain Management Group; Diabetes workshops for Year 6’s with Type 1 diabetes and their parents/Carers; Burns day and residential rehab. programmes outside of the hospital setting; Parent groups) - School-based transition and reintegration programmes
Waiting Times
We will try and see you and your child as soon as possible and we aim to offer an initial appointment within 4 weeks. The first appointment might be a triage telephone consultation that will enable to come with the best plan to support you and accommodate your needs.
We try to be as flexible as possible with appointment times. If you decide that your child no longer needs our services or that you do not wish to accept the appointment offered, please can you let us know as soon as possible so that your appointment can be allocated to someone else. If the appointment date/time is not convenient, please contact us and we will try to provide an alternative date/time.
Frequently Asked Questions
The Paediatric Psychosocial Service (PPS) is a specialist CAMHS team (Child and Adolescent Mental Health Service) for children and young people who are being treated at the Royal Manchester Children’s Hospital. We provide psychological and psychiatric assessment and treatment for patients who face emotional and mental health challenges related to their underlying physical illness.
The team consists of:
- Psychologists
- Neuropsychologists
- Psychiatrists
- Psychotherapists
- Mental Health Practitioners
- Secretaries and administrators
PPS can help support children and their families navigate treatment and manage living with a medical condition. They can also help people and families cope with the emotional impact of a serious or life-threatening illness or injury. Our neuropsychologists can help identify what someone is good at and where they might need help, and we can work with schools and others involved to make sure they get the right support. During your appointments, we will try to help you understand how your physical health might impact your mood, your relationships, your schoolwork, and the things you like to do, and help you find ways to enjoy your life despite having a health condition. This may be 1.1. with a professional, or in a group where you might meet other people who have similar challenges to you.
The Paediatric Psychosocial Department is not an emergency service. If you're in immediate distress, you can:
- Text “Shout” to 85258
- Call NHS 111
- Visit your GP or the nearest hospital Emergency Department
- Contact Childline at 0800 1111
- Call the GMMH 24/7 Help Line at 0800 953 0285
- Reach out to Papyrus Hope Line UK at 0800 068 41 41
Yes. It is our policy that family, relatives or friends cannot interpret for patients. Should you require an interpreter, ask a member of staff to arrange it for you.