Who are the Community Eating Disorder Service (CEDS)
The Community Eating Disorder Service (CEDS) is a specialist CAMHS community team (Child and Adolescent Mental Health Service), for children and young people aged 5 – 17 who may be presenting with an eating disorder or eating difficulties. We provide specialist evidence-based therapeutic interventions to young people and their families, through a range of treatments, as well as physical health monitoring.
MFT CEDS is split into two teams providing support for those with a suspected eating disorder and a specialist ARFID (Avoidant/restrictive food intake disorder) team. Our multi-disciplinary team includes Psychiatrists, Family Therapists, Advanced Clinical Practitioners, Specialist Dieticians, Occupational Therapists, CBT Therapists, Eating Disorder Practitioners, Paediatric Doctors, Nurses, Clinical Support Workers and Admin. We see our children and young people in a variety of settings along their journey which could include, our clinic bases, hospital, home based or a school setting. We aim to ensure the earliest, most effective intervention is offered.
Our team is diverse and inclusive, bringing together individuals from a variety of backgrounds, experiences, and identities. We’re dedicated to cultivating a culture that respects, values, and celebrates this diversity.
Our People:
Service Leads:
Dr David Ochando – Consultant Child and Adolescent Psychiatrist, Clinical Lead for MFTCEDS, CAMHS Clinical Director and GM Clinical Lead CYP Eating Disorders.
Molly Caine – MFT CEDS Service Lead
Emily Birch – ARFID and Neurodiversity Lead.
Psychiatrists:
Dr Meenaka Ramachandran – Consultant Child and Adolescent Psychiatrist
Dr Amy McCulloch – Clinical Research Fellow
Paediatrician:
Dr Dan Mattison – Consultant Paediatrician
Advanced Clinical Practitioners:
Rachel Coyle
Julie Milne
Family Therapists:
Karen O’Connor – Family and Systemic Psychotherapist
Sarah Hillman – Senior Eating Disorder Practitioner/Trainee Systemic Family Therapist
Karen Austin – Senior Eating Disorder Practitioner/Systemic Practitioner
Dietitian:
Ana Nikiforovski – Highly Specialist Dietitian
Eating Disorder Practitioners:
Vicky McGee – Senior Eating Disorder Practitioner
Rachelle Davies – Senior Eating Disorder Practitioner
Megan West – Senior Eating Disorder Practitioner
Freya Wheba – Senior Eating Disorder Practitioner, CBT Therapist
Sarah Findlay – Senior Eating Disorder Practitioner
Sarah Tritton – Senior Eating Disorder and ARFID Practitioner, Occupational Therapist
Jo Williams – Senior ARFID Practitioner, Occupational Therapist
Sharon Leah – ARFID Practitioner
Anna Beck – Eating Disorder Practitioner
Clinical Support Workers:
Mia Jackson – Clinical Support Worker
Raheema Hussain – Clinical Support Worker
Admin:
Jayne Cooke – Senior Medical PA, Senior Administrator
Susan Kedie – Team Secretary
Aisha Ahmed – Team Secretary
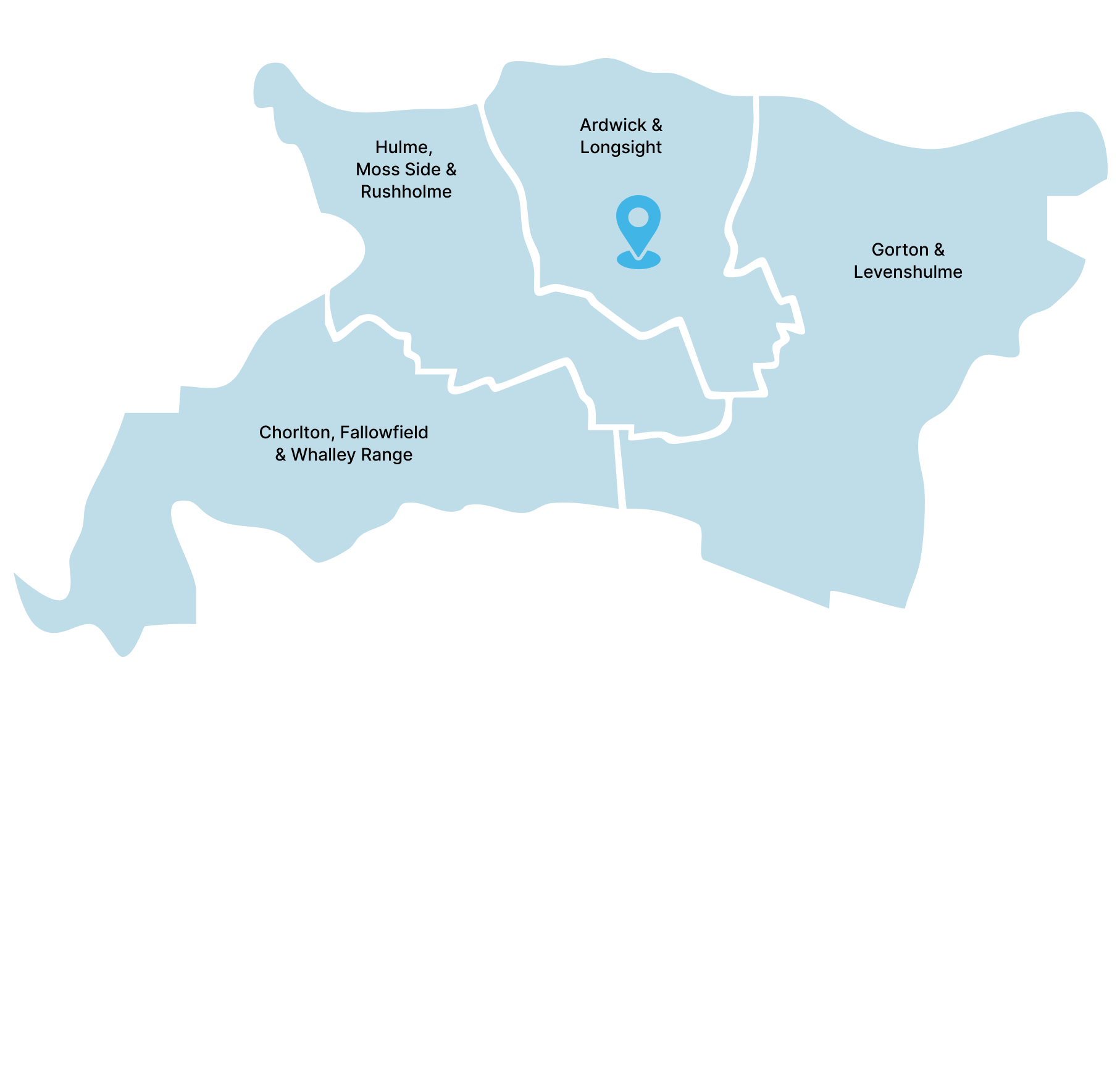
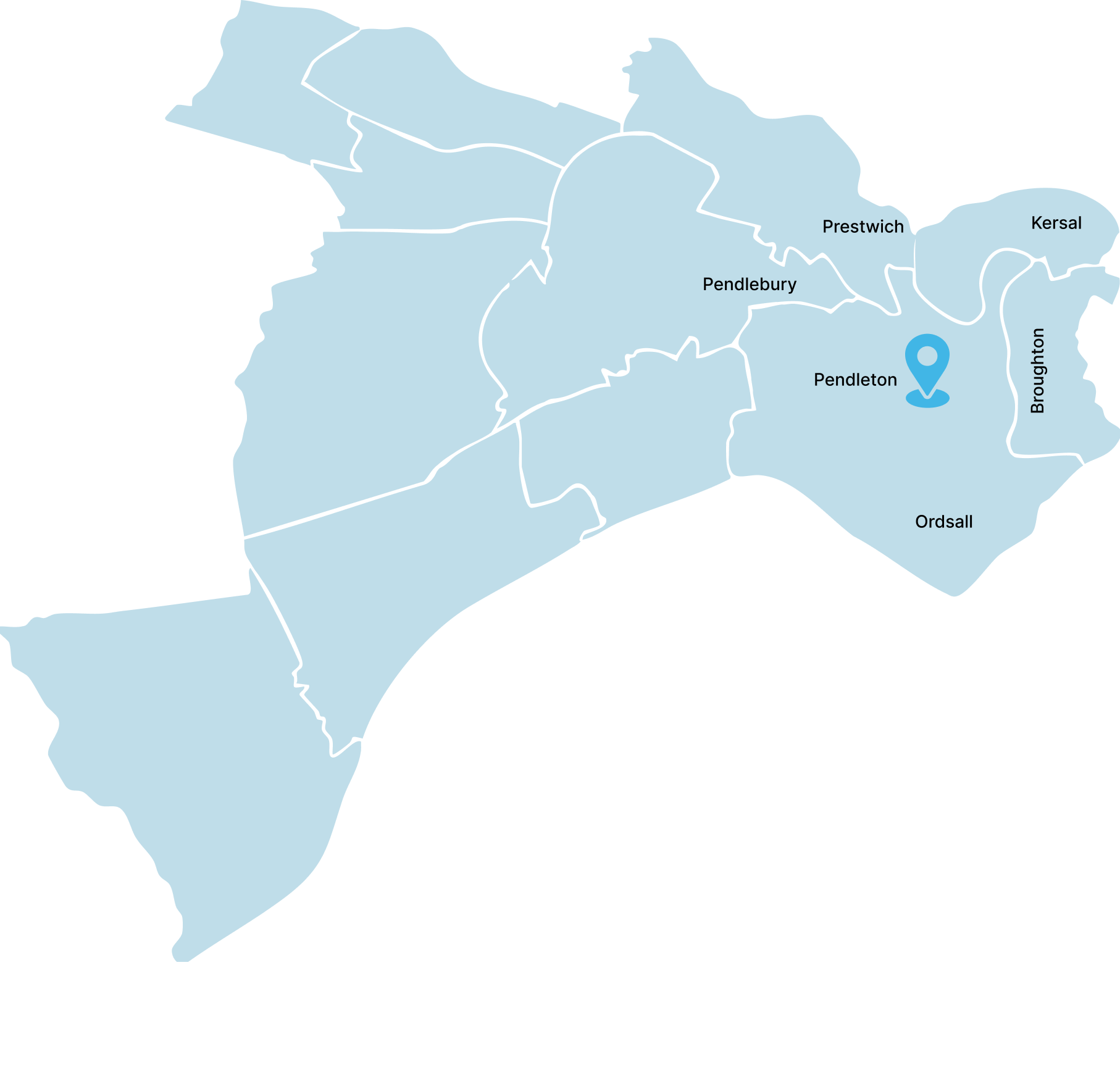
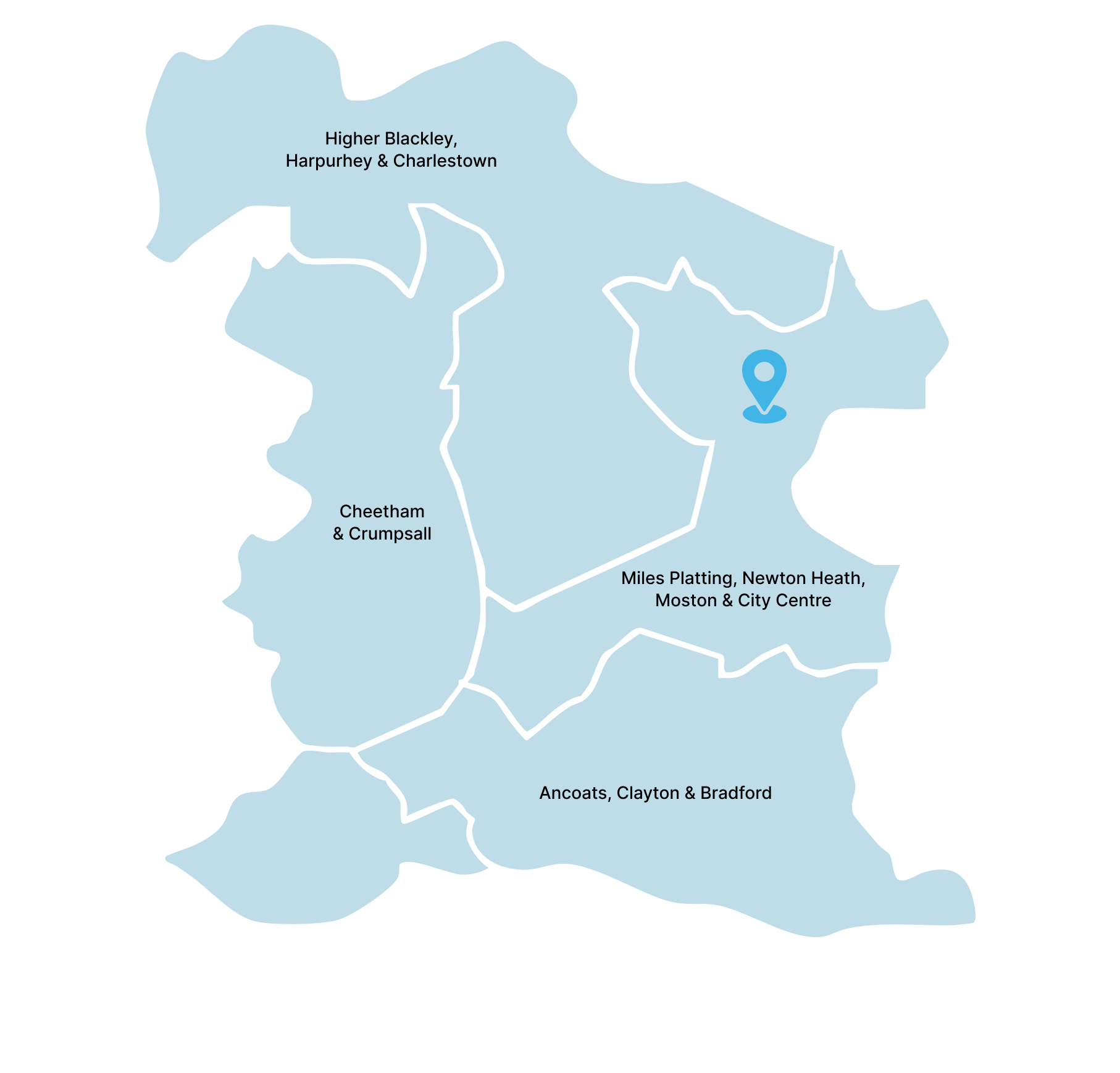
Community Eating Disorder Service Locations
How to get to us:
By bus: V1, V2
By train: The nearest train station is Manchester Oxford Road
How to get to us:
By bus: 101, 248, 249, 11, 368 Southmoor Road bus stop (~3 min walk) Opal House bus stop (~4 min walk)
By tram: Roundthorn Metrolink stop (~1min walk)
How to get to us:
By bus: 10, 35, 38, 50, 79 Salford Shopping Centre
By train: Salford crescent railway station (11 min walk)
How to get to us:
By bus: 114, 151, 688, 83, 84, 181, 182 Thorp Road bus stop (~2 min walk)
By tram: Central Park Metrolink stop
In need of urgent help?
Get Urgent Help NowAccess to CEDS
Navigating eating difficulties can be challenging, if you are experiencing eating difficulties and think you may need support, you or your family/carer can self-refer directly to our service. This can be done through calling us on 0161 701 0447 and requesting to speak with one of our practitioners, or alternatively you can email a summary to mftceds@mft.nhs.uk. This inbox is monitored Monday – Friday 9-5. Alternatively, you can fill out the referral form attached on this website, or receiving this after emailing mftceds@mft.nhs.uk
If you would like to access support for ARFID, this can be done through completing the referral form with a completed food diary. Both documents can be accessed through emailing mftceds@mft.nhs.uk or through this website. If you are wondering whether to refer a young person, please feel free to contact us using the above email address, or phoning 0161 701 0447.
With consent from the family or young person, we also accept referrals from:
- GP
- Health Professionals
- Social Care Professionals
- Anyone working with young people and families.
Waiting Times
We aim to screen all referrals the same day (Monday – Friday 9 – 5). Once a referral is screened, this will be taken to a weekly team meeting to collaboratively discuss the next best course of action. If it is determined to assess the young person, we see all our young people within four weeks of the referral being received, and within one week for those identified as urgent. If the referral is not accepted, we will inform the referrer of this decision.
The assessment process for CEDS includes:
- An initial face to face assessment appointment. This typically includes two of our practitioners meeting with the young person and their family, but there will also be an opportunity or option for the young person to speak with the practitioners on their own if preferred.
- The initial assessment is an opportunity to gather information around eating difficulties and assess what further support might be required or helpful. During this appointment, we will ask questions around your eating difficulties, to help us gain insight and understanding of how this is impacting your day-to-day life.
- We often will monitor your physical health during these assessments. This is done by measuring your height and weight and checking your blood pressure and pulse. Sometimes we may feel a blood test, or other medical investigations are necessary, and we would arrange this for a future date.
- We may also sometimes require permission to speak to other professionals involved with the young person, such as a school, or a GP.
- Following assessments, we take all of our assessments back to our MDT meetings which occur every Tuesday and discuss the assessment with a range of mental health professionals within the CEDS service, to think about what might best for our young people.
Waiting times within the ARFID team can look slightly different, and at current do not have a timescale for when young people will be seen. Referrals are only accepted by those with a Manchester, Trafford or Salford GP practice.
The assessment process for the ARFID team includes:
- An initial telephone assessment which involves speaking with one of our practitioners and asking further questions to gain an understanding of the young person’s eating difficulties, how long this has been ongoing for and what you feel the difficulties currently are.
- Following this we take all telephone assessments back to our MDT meetings which occur every Wednesday and discuss the assessment with a range of mental health professionals within the ARFID service and think about the next course of action for our young people, which could either be a further face to face assessment seen by two of our practitioners, or a telephone consultation.
Frequently Asked Questions
The Community Eating Disorder Service (CEDS) is a specialist CAMHS community team (Child and Adolescent Mental Health Service), for children and young people who may be presenting with an eating disorder or eating disorder difficulties. The Community Eating Disorder Service (CEDS) is split into two teams, those with a suspected eating disorder or eating disorder difficulties, and a specialist ARFID team. We provide specialist evidence-based therapeutic interventions to young people and their families, through a range of treatments, as well as physical health monitoring.
The team consists of:
- Psychiatrists
- Paediatricians
- Advanced Clinical Practitioners
- Nurses
- Occupational Therapists
- Family Therapists
- CBT Therapists
- Support Workers
- Admin Staff
CEDS can help support young people and their families navigate eating disorders and eating difficulties. We can also support individuals and their families in navigating the emotional and psychological impact of an eating disorder, helping them manage the challenges it poses to both health and daily life. We will help to identify during assessment and throughout treatment what evidence-based support may feel most beneficial in recovery. Support may be family focused, such as through family lens, focusing on a FT-AN approach, or through a 1:1 approach, or in a group setting where you might meet other people who have similar challenges to you.
The ARFID service can provide support through supporting young people and their families understand the different reasons behind the eating difficulties and support with building a toolbox of strategies that may help over time to bring around change. For primary and younger secondary school aged young people, there may be the option of a parent course in a group setting where you might meet other families who are experiencing similar challenges to you. For older teens, support may be offered through a 1:1 approach.
The Community Eating Disorder Service is not an emergency service. If you're in immediate distress, you can:
- Text “Shout” to 85258
- Call NHS 111
- Visit your GP or the nearest hospital Emergency Department
- Contact Childline at 0800 1111
- Call the GMMH 24/7 Help Line at 0800 953 0285
- Reach out to Papyrus Hope Line UK at 0800 068 41 41
Yes. Should you require an interpreter, ask a member of staff to arrange it for you, in advance of the appointment.