The HCC aims to standardise patient care across the North of England through the creation of over-arching HCC protocols which can be adapted for local use. These protocols are currently being developed and will be available for viewing in this section once completed.
National Guidelines:
Disclaimer: Guidelines available for download on, or linked to from, this website are for information purposes only and are not intended to inform any individual clinical decisions.
NICE Guidelines
This information will help guide and advise healthcare professionals with their health and social work. The National Institute for Health and Care Excellence have a platform which helps guide healthcare professionals to give the best care possible. The platform contains essential information for key groups including GP’s and public health professionals, it also contains resources to help maximise the use of evidence and guidance
There is an evidence search which helps you make better and faster evidence-based decisions and includes trusted resources from over 800 organisations. The evidence search helps to answer questions from both healthcare professionals and students. The platform helps you bring together evidence on health, drugs and technologies, public health, social care, and healthcare management and commissioning in one place.
The National Institute for Health and Care Excellence have a program called NICE Guidance which is there to give evidence-based recommendations developed by independent committees, including professionals and lay members, and consulted on by stake-holders. You can review the evidence across broad health and social care topics. There is also access to journals and databases where you browse or search for a particular journal, and then search for relevant articles within it. You can gain quick access to a range of journals and other evidence-based resources for health and social care staff in England.
These resources are provided in partnership with Health Education England and NICE and you’ll need an NHS Open Athens account to access most of these resources. For more information please see the following links
- Nice guidance on SCD
- Nice guidance – Sickle cell disease: managing acute painful episodes in hospital
- Nice guidance – Blood Conditions
- Nice guidance and advice
British Society for Haematology (BSH)
- Guidelines for the Management of Sickle Cell Disease in pregnancy
- Guidelines for the use of hydroxycarbamide in children and adults with sickle cell disease
- Red Cell Transfusion in Sickle Cell Disease Part I
- Red Cell Transfusion in Sickle Cell Disease Part II
- Management of Acute Chest Syndrome in Sickle Cell Disease
- Guidelines for the monitoring and management of iron overload in patients with haemoglobinopathies and rare anaemias
- The Use of Next-generation Sequencing in the Diagnosis of Rare Inherited Anaemias: A Joint BSH/EHA Good Practice Paper
Sickle Cell Society – Standards and Recommendations for Clinical Care Organisations
- Standards for Clinical Care of Adults with Sickle Cell Disease in the UK
2nd Edition, 2018 - Sickle Cell Disease in Childhood: Standards and Recommendations for Clinical Care
Executive summary Sickle Cell Disease in Childhood: Standards and
Recommendations for Clinical Care 3rd edition
North West HCC Sickle Cell Disease Network Protocols
All Network policies are reviewed and agreed by HCC Sickle Cell Board. Documents are subject to change to reflect changes in national practice / guidance.
Note that the annual review templates are for guidance and reflect the NHR data requests at the time of publication.
All templates provided can be altered to suit local population needs at the Consultants / Nurse’s discretion.
North England HCC Thalassaemia & Rare Inherited Anemia Network Protocols
All Network policies are reviewed and agreed by HCC Thalassaemia & RIA Board. Documents are subject to change to reflect changes in national practice / guidance.
Note that the annual review templates are for guidance and reflect the NHR data requests at the time of publication.
All templates provided can be altered to suit local population needs at the Consultants / Nurse’s discretion.
- Annual Review Template – Adult Non-Reg Transfusion
- Annual Review Template – Paediatric Non-Reg Transfusion
- Annual Review Template – Adult Regular Transfusion
- Annual Review Template – Paediatric Regular Transfusion
- Standardised Transfusion Care Plan Template – pending
- Adapted Royal College Nurse Competencies Framework Thal & RIA
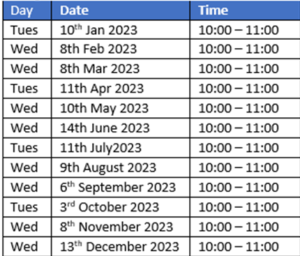
North West England Sickle Cell HCC Specialist MDT
This clinical multiple disciplinary team (MDT) is a subgroup of the North West England Sickle Cell haemoglobinopathy coordinating centre (HCC) led by Manchester University NHS Foundation Trust.
The clinical MDT aims to ensure optimal and consistent care is provided to haemoglobinopathy patients within the region in line with national and regional standards.
The MDT provides a forum to discuss and review patient care, and report/discuss serious incidents and similar investigations.
The MDT provides a forum for shared learning including expertise from clinicians specialising in the relevant areas.
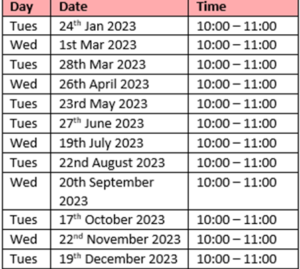
North England Thalassaemia & RIA HCC MDT
This clinical multiple disciplinary team (MDT) is a subgroup of the Northern Sickle Cell and Thalassaemia Alliance (NOSTA) led by Manchester University NHS Foundation Trust, the designated haemoglobinopathy coordinating centre (HCC). For governance purposes, this meeting reports to the NOSTA Steering Group.
The Clinical MDT aims to ensure optimal and consistent care is provided to Haemoglobinopathy Patients within the region, in line with national and regional standards.
The MDT provides a forum to discuss and review patient care, and report/discuss Serious Incidents and similar investigations.
The MDT provides a forum for shared learning.
Dates
National Haematology Registry (NHR)
The National Haemoglobinopathy Registry (NHR) is a confidential database of patients with red cell disorders living in the UK. All patients with sickle cell disease, thalassaemia, and rare inherited anaemias such as Diamond Blackfan anaemia, sideroblastic anaemia, red cell enzyme disorders are included. Patients with these disorders are managed by specialised haemoglobinopathy services and teams (SHT.)
The aim of the registry is to improve patient care by ensuring clinically important information related to patients’ health, treatment and complications is available to SHTs who are involved in the patient’s clinical care.
The registry merges clinically important information about patient’s health which is already available on different databases and hospital records into one central database to ensure relevant and important information is in one place. This means that if the patient needs treatment at another centre important parts of patient’s health record is available to the team providing urgent care.
Information from the NHR, helps NHS England understand the specific needs of people with haemoglobin disorders so that they can assess the quality of services and help guide future funding from the commissioners for specialist haemoglobinopathy centres. This is an important process in improving access to treatments in your local haematology centre. This information is also essential for healthcare planning, identifying accurate patient numbers and conducting research into areas such as patient experience, quality of care, timeliness of care.
Useful documents for GPs
Our Haemoglobinopathy Carrier States (Genetics) Information Leaflet for Health Professionals provides an overview of what haemoglobinoapthies are, symptoms and information regarding investigations and referral.
Key Points
- Carriers for haemoglobinopathy do NOT usually require haematological referral or follow-up
- Refer if anaemia > 20g/l below normal range or splenomegaly or symptoms and iron deficiency excluded
- Blood counts for an individual tend to remain stable in adults so investigate if Hb drops from usual steady date
- Consider if genetic counselling information is needed
- Further advice and patient information can be obtained from the Manchester Sickle Cell and Thalassaemia Centre – 0161 279 3322
No One’s Listening Report, November 2021
An All-Party Parliamentary Group (APPG) inquiry report (published November 2021) highlighted failures of care for sickle cell patients in secondary care.
The ‘No One’s Listening’ report, which is based on the inquiry’s findings, is jointly published by the APPG on Sickle Cell and Thalassaemia and the Sickle Cell Society, a national charity that supports and represents people affected by sickle cell disorders.
As a result of the report, NHS England requested Trusts to respond to the recommendations outlined in the document. To read your local haematology teams response, contact your local team / regional HCC Lead.
Can you tell it is Sickle Cell?
Overview
NHS England and NHS Improvement is continuing it’s Sickle Cell awareness campaign ahead of World Sickle Cell Day 2023.
Objectives/Aims
The campaign, which is part of a bigger drive to improve sickle cell care across the NHS, aims to increase awareness of the key signs and symptoms of a Sickle Cell crisis, particularly among urgent emergency care staff and those living with the condition and their carers.
It also aims to promote and generate uptake of a new e-learning module about the condition and the healthcare inequalities related to it.
You can access NHS England Can you tell it’s Sickle Cell? comms toolkit here
 In this section
In this section