ABPA – Allergic Broncho-Pulmonary Aspergillosis
ABPA is estimated to affect 2.5 – 5% of those people with bronchial asthma, which equates to 125,000 – 250,000 cases, though the number diagnosed is far lower. Much better diagnostics are needed! Diagnosis can be very slow, with some estimates giving an average of 10 years (and up to 20 years) between the first symptoms and final diagnosis, a claim which is certainly borne out by the comments of some existing ABPA patients.
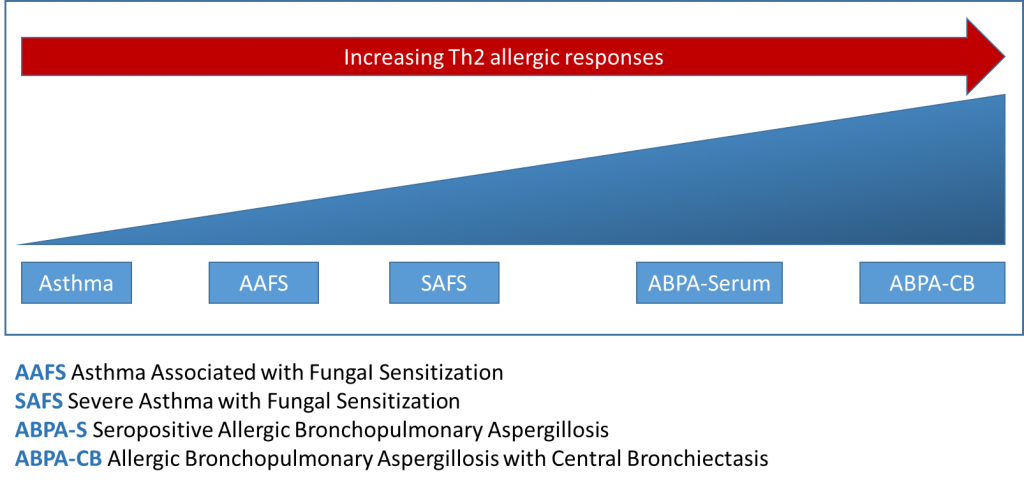
Allergic broncho-pulmonary aspergillosis is a condition that causes the patient to develop an allergic response in the airways to Aspergillus spores or colonising Aspergillus moulds. ABPA is predominantly found in patients with treatment-resistant asthma (although this is not always the case) and cystic fibrosis, and manifests with transient and fleeting pulmonary opacities and bronchiectasis.
Typically ABPA is predominantly associated with poorly controlled asthma but can also include excessive mucus production, mucous plugs, coughing, haemoptysis, bronchiectasis, low-grade fever, weight loss and malaise.
ABPA is initially managed using oral steroids to suppress the overactive immune response in an attempt to prevent the disease from progressing to bronchiectasis – if detected early enough bronchiectasis can be delayed or even avoided. Antifungals (e.g. itraconazole) can be useful to help minimise the dose of oral steroid while at the same time controlling asthma symptom exacerbation.
Typically the fungus can be observed histologically growing in lung airways, albeit sparsely but it seems likely that incoming spores as the patient inhales also contribute to the fungal load. The fungus does not invade the lung tissue itself (it is non-invasive) but sets up a permanent source for irritation and allergic reaction. Sufferers of ABPA find anywhere that has increased levels of airborne mould spores can trigger severe asthmatic reactions – e.g. compost heaps, damp buildings. Avoiding exposure can help reduce symptoms.

Diagnosis
The ISHAM-ABPA working group has proposed criteria, published in 2013. However, there have since been modifications of the criteria to enhance their sensitivity:
Predisposing conditions |
| Asthma, cystic fibrosis |
| Obligatory criteria (both should be present) |
| Immediate cutaneous hyper-reactivity to Aspergillus antigens or Aspergillus fumigatus-IgE >0.35 kUA/l |
| Total IgE >1000 IU/ml |
Other criteria (at least 2 out of 3) |
| Peripheral blood eosinophil count >500 cells/µl |
| Transient pulmonary infiltrates on chest radiograph |
| Presence of precipitins (IgG) against A. fumigatus |
ISHAM-ABPA Working Group diagnostic criteria for ABPA (suggested modifications) |
Predisposing conditions |
| Asthma, cystic fibrosis |
| Obligatory criteria (both should be present) |
| A. fumigatus-IgE >0.35 kUA/l |
| Total IgE >1000 IU/ml |
Other criteria (at least 2 out of 3) |
| Peripheral blood eosinophil count >500 cells/µl |
| Bronchiectasis on computed tomography of the chest |
| A. fumigatus-IgG >27 mgA/l |
Source: Agarwal et.al. 2020, adapted with permission from Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopulmonary aspergillosis: Review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43:850–73.
ABPA in special situations and related conditions
Agarwal et.al. 2020 goes into more detail on the following:
- In children
- During pregnancy
- ABPA complicating cystic fibrosis
- ABPA in non-asthmatic patients
- ABPA complicating other conditions e.g. bronchiectasis, post-tubercular lung disease, Kartagener’s syndrome, Macleod’s syndrome, chronic obstructive pulmonary disease, chronic granulomatous disease and hyper-IgE syndrome
- Allergic bronchopulmonary mycosis (Non-Aspergillus fumigatus cases)
- Sinobronchial allergic mycosis i.e. Patients with ABPA can have coexistent allergic fungal rhinosinusitis (AFRS)
Treatment
Treatment consists of long term use of oral steroids (e.g. prednisolone) to reduce inflammation and lung damage. There are several potential difficulties with the use of steroid drugs for long periods but their use is vital to prevent the disease from progressing.
When steroid dose is high and starts to cause significant side effects we can also often reduce the quantity of steroids taken by ABPA patients by giving the patient an antifungal medication such as itraconazole. This seems to keep the inflammation under control.
Omalizumab can be an effective treatment for ABPA, though it is not funded for this use by the NHS (Patel et.al. 2019 Treating Allergic Bronchopulmonary Aspergillosis: A Review).
Prognosis
There is no complete cure for ABPA, but management of the condition usually succeeds in stabilising the symptoms for many years.
ABPA can rarely progress to CPA.
Allergic Fungal Rhinosinusitis (AFRS)
AFRS is a chronic condition that can be difficult to manage and can be highly debilitating with significant loss of quality of life. Patients generally have all of the following: immunocompetence, eosinophilic mucin containing noninvasive fungal hyphae, nasal polyposis, specific radiographic findings, and allergy to cultured fungi.
AFRS can present with gross facial distortion, sinus blockage and even loss of vision or alternatively and more commonly they can have no outward signs.
Diagnostic criteria for sinusitis have been defined by consensus in Meltzer EO et al. 2004 as follows:
| Symptoms | Requires ≥ one of the following: |
| • Anterior and/or posterior nasal drainage | |
| • Nasal obstruction | |
| • Decreased sense of smell | |
| • Facial Pain-pressure-fullness | |
| Objective findings | Requires all of the following: |
| • Presence of allergic mucin (pathology showing fungal hyphae with degranulating eosinophils) | |
| • Evidence of fungal specific IgE (skin test of in vitro test) | |
| • No histologic evidence of invasive fungal disease | |
| Radiographic findings | Highly recommended: |
| • Sinus CT demonstrating | |
|
|
|
|
|
|
|
|
| Other diagnostic measures | Possible, but not required: |
| • Fungal culture | |
| • Total serum IgE | |
| • Imaging by more than one technique( CT or MRI) |
Treatment
Management of AFRS requires repeated surgical debridements, correction of any immunologic deficiency, and long-term systemic and topical antifungal therapy. Despite close medical attention, all invasive cases of fungal rhinosinusitis can progress to a fatal outcome or become a recurrent problem.
Further Information
 In this section
In this section