This page provides information for GPs for our Rheumatology service at Wythenshawe, Trafford, Withington, and Altrincham hospitals
Contact us
We available for telephone advice Monday- Friday 9am-5pm. Please contact the switchboard at Wythenshawe hospital and ask for the STR or Consultant on call for Rheumatology. At weekends there is also a Consultant available for telephone advice.
We are happy to discuss any cases, particularly if there is clinical urgency or diagnostic uncertainty for example a patient with atypical giant cell arteritis. Please note that patients should also be referred electronically via Gateway or ERS depending on your locality.
Referrals
We triage referrals daily on weekdays.
What and how to refer
Please see patients face to face and include examination findings where relevant e.g. suspected inflammatory arthritis. Patients with suspected connective tissue disease or vasculitis need to have a urine dipstick and blood pressure as well as a face to face examination recorded prior to referral. Incomplete referrals will be returned for more information.
The full scope of conditions which should be referred to Rheumatology is available on our directory of services. This includes suspected inflammatory arthritis including axial spondyloarthritis, suspected autoimmune connective tissue disease, small or large vessel vasculitis including giant cell arteritis (if there is visual involvement patients should also be referred to Ophthalmology same day as an emergency), gout (consider A and G for queries), polymyalgia (consider A and G for queries), osteoporosis (patients aged 70 or over should be referred to the complex health bone clinic) and Paget’s disease.
EIA
It’s worth noting that criteria for our suspected early inflammatory service are as follows. Referrals which meet these criteria will be fast tracked.
EIA service criteria are 3 or more of the following:
- Recent onset of swollen joints < 6 months
- Symptoms worse in the morning with > 30 minutes of early morning stiffness
- Pain on squeezing knuckles/ PIPs/ toes
- Joint symptoms responding to NSAIDs
- Raised inflammatory markers (ESR or CRP )
- Positive CCP +/- rheumatoid factor
- Swollen small joints of the hands and or feet (on examination by a doctor)
GCA
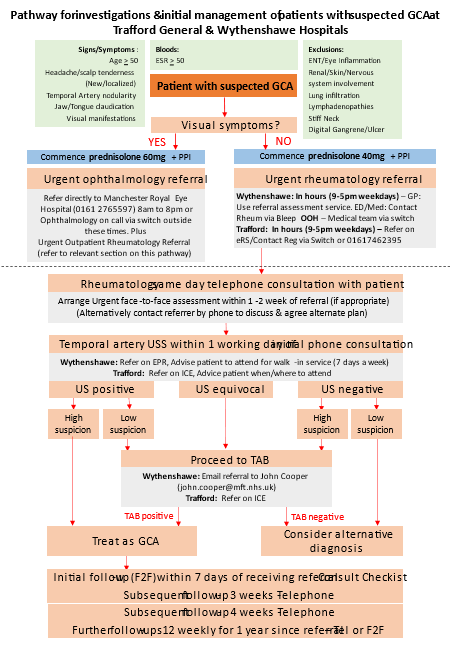
Details of our GCA pathway can be found below. Please do contact us to discuss cases if helpful. You also need to refer electronically. Make sure you start prednisolone when indicated and refer urgently.
Who not to refer
- We will return referrals of patients who are suspected to have a non-inflammatory condition in line with guidance from the British Society of Rheumatology.
- Please do not refer; suspected cancers including bone malignancy, suspected cauda equina syndrome, patients with positive antibody results in the absence of symptoms, osteoarthritis, fibromyalgia, chronic fatigue syndrome, hypermobility.
- Patients who have been diagnosed with fibromyalgia and need advice about pain management should be referred to the pain clinic.
- Patients with suspected chronic fatigue syndrome should be referred to Endocrinology.
- Please do not refer patients with long COVID unless they have symptoms and signs suggestive of inflammatory arthritis or connective tissue disease.
Fibromyalgia
Many people living with fibromyalgia syndrome (FMS) can be diagnosed and managed in primary care and a referral to secondary is not routinely required. Further guidance on the diagnosis of FMS, including a 1 page summary and FMS diagnostic worksheet to complete with the patient, is available in the UK FMS diagnosis guidelines here. A patient information leaflet about FMS is available here Fibromyalgia | Causes, symptoms, treatment | Versus Arthritis.
We are content to review patients with possible FMS to confirm the diagnosis where there is a concern that other inflammatory conditions need to be excluded. If this is the case, please refer highlighting the features present which may suggest an alternative diagnosis to enable us to safely triage the referral. Please note there may be a significant delay in the patient being seen and adoption of a pain management approach in primary care in the interim may be appropriate. Where a diagnosis of FMS is confirmed, the patient will be discharged back to primary care for further management.
FMS is a form of chronic primary pain and we would endorse the management recommendations in the NICE Chronic pain guidelines NG193. We would highlight there are a range of healthcare professionals available in primary care including FCPs, social prescribers and pharmacists who can also provide support to people living with FMS.
A referral to the rheumatology service does not provide access to any specialist services which are not otherwise available from primary care. People living with FMS, who following optimisation of a pain management approach in primary care, continue to experience significant symptoms may benefit from a referral to the pain service.
Hypermobility
The majority of patients with hypermobility spectrum disorders (HSDs) or hypermobile Ehlers Danlos syndrome (hEDS) can be managed in primary care. There may not be much advantage for an individual patient being reviewed within a general rheumatology clinic. A referral simply for confirmation of a diagnosis is not routinely recommended, and due to the high volume of inflammatory disease may result in a long wait.
The Ehlers Danlos GP toolkit (available here The Ehlers-Danlos syndromes (EDS) GP Toolkit) provides helpful referral guidance.
If any hypermobile condition other than hEDS/HSD is suspected (see referral guidance above) then a direct referral to clinical genetics in the first instance may be appropriate.
The management approach for HSDs and hEDS focusses on the addressing the specific difficulties an individual experiences. For MSK symptoms physiotherapy, occupational therapy and podiatry may be helpful in the first instance. These services are available via the Tier 2 MSK service and this is usually significant quicker than being seen in the rheumatology service.