- Arranging semen analysis appointments
- Arranging semen analysis without an electronic request
- Retrograde semen analysis
- Sample acceptance policy
- Specimen containers
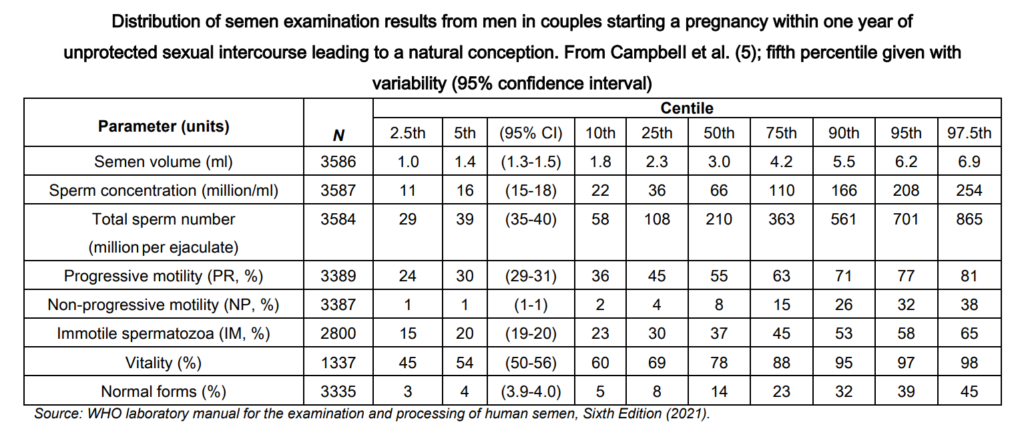
- Reference ranges
- Measurement uncertainty values for semen analysis
- Turnaround times
- Information for patients
- Factors that may affect semen analysis results
Arranging semen analysis appointments
All requests for semen analysis should be made electronically by the requesting healthcare practitioner using the lab requesting system. Most appointments are for patients to pass the sample is one of our private rooms.
For surgeries that wish the patient to pass a semen sample in one of our private rooms (or if surgery has no packs) : Request ‘I want to collect sample later’ and print out a postponed summary. This summary should be emailed to mft.andrology@nhs.net and we will then send the patient an appointment.
Can samples be passed at home?
Yes, but an electronic request must be made and an appointment is required to drop the sample at the laboratory within 50 minutes of passing the sample. We understand that this may be difficult, but any samples received after this time could possibly lead to us requesting a repeat sample. Your referrer will be able to inform you if this is the case.
Some GP surgeries have our semen analysis packs. If not, patients can arrange to collect one from us (once the test has been ordered) by emailing mft.andrology.lab@nhs.net.
These samples need to be kept as close to body temperature as possible, so please ensure the patient understands that they need to keep their sample close to their body (in an inside coat pocket).
If you have any questions, please email mft.andrology.lab@nhs.net.
Please note that appointments cannot be given to patients over the telephone without a request having been received in Andrology.
The patient must bring the specimen directly to Andrology reception in the Department of Reproductive Medicine, Old Saint Mary’s Hospital on Oxford Road, Manchester, M13 9WL (if using Sat Nav enter post code M13 0JH), at their appointment time. They will need to press the bell at the window for a member of the team to receive their sample.
Retrograde semen analysis
Retrograde ejaculation is a condition where semen is ejaculated backwards into the bladder. This can be variable in severity and is associated with particular health conditions (such as diabetes) or if certain medications are being taken (such as alpha blockers). In cases where this is suspected, the urine is examined for the presence of spermatozoa, if there are no spermatozoa in the semen sample or if no semen is produced.
If this test is required, more specific direction will be given to you for this test. This will need to be booked on-site.
Sample acceptance policy
It is desirable that samples are labelled with four unique identifiers but mandatory that samples are labelled with at least three unique identifiers which are as follows :
- Surname
- Forename
- Date of birth
- Medical Record Number (MRN)
- NHS number
The request form data MUST match the above information on the sample. Where the sample is repeatable/ reproducible, no analysis will be performed and the sample will be discarded. A repeat sample will be requested. Andrology will accept no responsibility for analysed samples which initially failed to meet the acceptance criteria and will issue a disclaimer on such reports.
A lack of patient or sample information may result in the laboratory not conducting the analysis/ examination. Examples could include :
- No dates and times of sampling
- Location for report delivery not given
Request forms SHOULD also contain :
- The patient’s location/ destination for the report (or a location code)
- Tests required
- Name of Consultant or GP
- Name of the requester and contact number (bleep or extension)
- Date and time of sample collection
- Type of sample
- All relevant clinical information
- Patient address for GP requests
There may be some instances outside of the above information which may lead to sample rejection. If you are concerned, please talk to an Andrologist when you attend.
Specimen containers
Some plastics are toxic to sperm and can affect sperm motility. Andrology provide specimen containers that have passed toxicity testing and are suitable for semen specimens.
Reference ranges
Reports show reference values from the WHO guidelines 2021. Lower reference limits (5th centiles and their 95% confidence intervals) for semen characteristics:
| Parameter | Lower reference limit |
| Semen volume (ml) | 1.4 (1.3-1.5) |
| Total sperm number (million per ejaculate) | 39 (35-40) |
| Sperm concentration (million per ml) | 16 (15-18) |
| Progressive motility (PR, %) | 30 (29-31) |
| Sperm morphology (normal forms, %) | 4 (3.9-4.0) |
| Vitality (live spermatozoa, %) | 54 (50-56) |
| pH | ≥ 7.2 |
It is important to understand that this test can support healthcare practitioners understand how the reproductive system is functioning in the production of gametes (sperm) in patients that were assigned male at birth. Generally, the test is not considered a marker of fertility/infertility, but can give vital information that supports management pathways or ways to improve sperm quality.
For the distribution of values for semen parameters from men whose partners became pregnant within 12 months of discontinuing contraceptive use can be found in the WHO guidelines (see below).
Measurement uncertainty values for semen analysis
Every measurement is subject to some uncertainty. Measurement uncertainty can come from the measuring instrument, from the item being measured, from the environment, from the operator and from other sources. Measurement uncertainties can be estimated using statistical analysis of a set of measurements. The use of good practice such as traceable calibration, careful calculation, good record keeping, and checking can reduce measurement uncertainties.
In order to provide a measure of confidence in results produced by a laboratory, it is necessary to identify all factors which may contribute to variation of measurement in a process and assess the potential to influence uncertainty. Once identified these factors must be reduced or controlled to an acceptable level and a value for the range of acceptable uncertainty assigned where possible.
Andrology has determined the measurement uncertainty values for semen analysis. They are reviewed regularly and reassessed whenever a significant change in the procedure occurs, e.g. new equipment or modification of the assay.
These uncertainty measurement values are available upon request.
Turnaround times
Diagnostic semen analysis (GP referrals):
- 7-10 working days from receipt of specimen.
Diagnostic semen analysis (Department of Reproductive Medicine):
- The results will go back to the healthcare professional looking after you and provided at follow-up
Information for patients
There is a patient information leaflet: Diagnostic Semen Analysis.
A semen analysis is usually advised if a couple are having difficulty conceiving (becoming pregnant). Primary infertility is an extremely common problem, affecting more than one in seven couples attempting their first pregnancy. Among those experiencing difficulty with conception, a male fertility problem is considered important in around 40 per cent of couples.
The sample will be analysed according to the World Health Organisation (WHO) guidelines for volume, pH, concentration, motility, viability and morphology. Results are sent to the referring doctor within 5 working days of the semen analysis.
Factors that may affect semen analysis results
- Some plastics are toxic to sperm so specimen containers must be obtained from Andrology as these have been tested for toxicity.
- Extremes of temperature can damage sperm so the sample should be kept at body temperature whilst being transported to the laboratory, for example by carrying it in an inside pocket.
- A condom and/or artificial lubrication must not be used for semen collection, as it will kill the sperm.
- Motility of sperm can decline over time so it is important that the semen sample is examined within an hour of it being produced.
- The sperm ‘rich’ fragment of an ejaculate is considered as the first part produced, so the whole of the specimen should be collected to support adequate interpretation. We will not reject your sample if this is not the case, but it does help us understand how to interpret the results.
- The number of days of sexual abstinence can affect the quality of sperm.
- Abstinence should be between 2 – 7 days (3 or 4 days is best) for semen analysis.
- Viscous specimens or specimens where there is sperm agglutination can affect semen analysis results.
- Past medical history may be important in understanding where there may be reduced sperm quality, such as cancer treatment or previous infections.
- The use of medications prescribed by a healthcare professional (we do not advise stopping medications, just ensure that if you talk to the person who referred you when you discuss results or ask to speak an Andrologist)
- The use of ‘recreational drugs’ which can be anabolic steroids, exogenous testosterone, cannabis etc. Please talk to the person who referred you or ask to speak to an Andrologist regarding this.
There may be occasions where we refer you back to the person who referred you, this is only due to them having a comprehensive medical history.
 In this section
In this section