The Laboratory Medicine Care Division (LMCD) guidelines for specimen acceptance must be followed to ensure that all samples are correctly and unambiguously identified. The policy provides an overarching process to specimen rejection to help balance the requirement to process against the risk to patient safety. Clinical governance issues may arise from errors in specimen identification and/or insufficient clinical information being given with a specimen. To ensure that specimens are linked to the correct patient, adequate identifiers are essential. Due to the difficulty in repeating a tissue specimen, different criteria are used in Adult Histopathology.
All urgent and specimens on a cancer tracking pathway (HSC205) should be clearly labelled as such. The date and time the specimen was taken is important information that should be included on all requests to determine the length of fixation of the tissue specimen.
TopSpecimen Acceptance Policy
All samples sent to the laboratory must comply with our specimen acceptance requirements and be accompanied by a correctly completed histology request form. For test requests ordered on the Hive Electronic Patient Record (EPR) system. For non-Hive requests, samples sent from an External source or paper requests raised during Hive downtime, the following mandatory information must be provided for us to accept the specimen:
Essential Patient Identifiers:
- Surname
- Forename
- Unique identification number – Medical Record Number (MRN), NHS or external hospital number for external cases
- Date of birth
- Address – for external locations
Essential Clinical Details:
In producing a final diagnostic histopathology or cytopathology report the Pathologists are essentially looking to provide guidance and answers to clinical queries. Therefore it is essential that all relevant clinical information is provided on the request form (paper based or electronic) so that the histological features of the specimen can be interpreted within the clinical context. Rather than simply repeating oneself under each heading give relevant clinical details, procedure details, medical history and the clinically suspected (differential) diagnosis. This should include all previous malignancies, whether in the same or any other organ system. Under Specimen Details, give the precise anatomical site of the specimens sent. If there are multiple specimens, there should be a one-to-one correspondence between the specimens listed on the card and the labelling of the specimen pots. State any markers / sutures / clips, and their significance. Record any features of the specimen that are likely to be difficult to interpret after fixation, particularly for complex resections.
If the relevant, appropriate clinical information is not provided this may lead to a delay in the final report being issued.
- High risk of infection status – to ensure health and safety of all staff
- Specimen site – must match on specimen pot and request card
- Relevant clinical information – to ensure all necessary investigations are performed, gestation date and LMP for gynaecological specimens
- For Lung cancer – any sample where there is a clinical concern for lung cancer (primary or metastatic), please ensure details of smoking (never/light smoker or current/ex-smoker) and performance status (WHO 0 1 2 3) are recorded on the request form in the clinical details section.
- Consent – fully completed PS1 form and gestation date or LMP for early pregnancy tissue specimens, with clear indication of cremation or burial wishes.
- Date/time taken – essential to ensure proper fixation of high risk specimens
Essential Sender Details:
- Ward/department – required for return of external reports
- Consultant or GP – required for return of external reports and contact in case of any errors/discrepancies
- Contact number/bleep – for frozen sections
Specimens that do not contain the required information or have discrepancies between the request card and specimen pot will not be processed in the laboratory until the necessary information has been obtained. The sender will be contacted via email or instant messaging on Hive (internal MFT only) to rectify any problems. In the event the sample is unrepeatable, the department has protocols in place to deal with specimens/request forms that do not meet the specimen acceptance criteria however, a final report will not be issued until such details have been corrected.
If the discrepancy cannot be rectified by email or instant messaging or the changes are too substantial the sender will be asked to attend the laboratory to rectify the issue.
The person correcting the patient or specimen details should be of appropriate seniority and able to take responsibility for the labelling of the specimen. This will result in a delay to specimen processing and reporting.
Any high-risk specimens should be highlighted on the specimen request form and received in formalin. The specimen will be left to fix in formalin for 24 – 48 hours after receipt to ensure safe to handle and therefore there may be a delay in the report being issued.
TopRequest cards
All paper request cards should be completed in full (see above) and all information provided should be clearly legible. Any missing information or errors will result in a delay to specimen processing and reporting.
Correct patient and specimen information is vital for us to provide a quality service to our users. Any specimens deemed to be high risk or potentially high risk should be clearly labelled as such to protect the health and safety of all staff.
As we provide our service to a range of service users, please also state the type of unique patient identification number given, e.g. NHS, Medical Record Number (within MFT). Please also indicate whether the patient is an NHS, private or waiting list initiative patient.
If a patient is part of a research project, this should be clearly labelled on the request card to ensure that the specimen undergoes the correct procedures. Similarly, patients that are part of a screening programme, e.g. BCSP BOSS, should be clearly labelled.
TopHIVE requests
Unlike some of the other pathology disciplines. Cellular Pathology (Histology) still require a request card for specimens requested on HIVE>
For test requests ordered on the Hive Electronic Patient Record (EPR) system an order requisition printout must be submitted with the request.
HIVE generates specimen labels for both the requisition printout and each sample pot created as part of the order entry. Please ensure the correct label is attached to the correct container. HIVE labels must be attached to the specimen container and not to the lid of the container.
TopSpecimen containers and storage of specimens
Labelling multiple samples from the same patient
If there are multiple samples from the same patient from different sample sites or multiple samples from the same site:
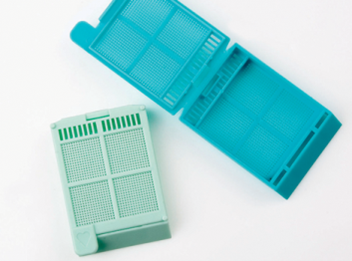
- Ensure each sample is collected in the appropriate sample collection pot (see Specimen Acceptance Policy)
- Ensure each pot is fully labelled with all the appropriate patient demographic information
- (see Specimen Acceptance Policy) – for HIVE orders each pot should have a unique sample label generated
- Ensure each pot is labelled with the specific sample source location i.e. skin lesion left arm
- If there is more than 1 sample/pot for a specific sample source location label each pot numerically, in the order they were taken.
Most specimens for histology need to be placed in an appropriately sized container with adequate amount of formalin (ideally 10x the volume of the sample) as soon as removed from the patient. Specimen containers of all sizes, pre-filled with formalin, are available from histology, please contact the laboratory. For specimens to be sent to the department not in formalin, empty specimen containers of all sizes are also available.
Prior to transport to the laboratory, it may be necessary to temporarily store specimens. All specimens that are placed into Formalin should be kept at room temperature until transported to the laboratory. Specimens in Formalin should not be placed into the fridge as this will have a negative impact on fixation and therefore preservation of the tissue.
| Specimen | Storage |
| Formalin | Room temperature |
| Dry unfixed | Fridge |
| Zeus medium | Room temperature |
| Gel transport medium | Fridge |
| Michel’s transport medium | Fridge |
| Gluteraldehyde | Room Temperature |
All dry specimens and specimens in gel transport medium ideally should be transported to the laboratory immediately. Where this is not possible, these specimens should be stored in the fridge. Specimens in Zeus medium should be stored at room temperature. Zeus medium should ideally be stored in the fridge prior to use.
TopTransport of specimens
Specimens for histology are not allowed to be transported via the pneumatic tube system.
The transport of hospital specimens to the department is undertaken by the respective hospitals transport portering teams. Dependent on the site, dedicated transport boxes/packaging will be used to deliver the specimen pots to the laboratory. Urgent samples, e.g. transplant biopsies, frozen sections, may be delivered to the department ad hoc; these should be transported in an appropriate container, with a tightly fitting lid. The transport containers should be labelled as Diagnostic Specimens – UN3373 and have the department name and telephone number to ensure the containers comply with transport regulations.
All specimen pots should be tightly sealed and transported using specimen bags, where appropriate. The request card if included should be placed in the pocket of the specimen bag, and the pot inside the sealed bag to ensure the safety of all staff. All specimens should be received with a documented tracking sheet detailing patient identifiable information such as specimen type and where the specimen has been taken. These tracking sheets are checked on arrival in the histology department and returned to the porter, department or area the specimen was taken from for staff to record that the specimen has been received safely in Histology.
There is also a transport pathway system for the transfer of specimens between MRI, Trafford General Hospital and Wythenshawe Hospital as well as Transport between Wythenshawe Histopathology, Withington Community Hospital, and Oxford Road Campus. These specimens should be sent via a packing list on Hive so they can be accepted by histology reception staff for audit and tracking purposes.
Transport of the Tameside samples occurs twice daily. The transport collects specimens from theatres, endoscopy and then pathology before leaving pathology at 9.30 am and 3.30 pm. This transport also delivers samples from GP surgeries within the Tameside borough. This transport also delivers supplies from MFT back to Tameside for the relevant theatres and clinics.
For specimens received from hospitals where there is not a routine transport service arranged, a courier service is used.
Samples from the GP surgeries within the South Manchester District are delivered to the main pathology reception area at Wythenshawe and then collected by histology staff on an ad hoc basis. Some of these samples are requested electronically others are accompanied by handwritten request forms. For paper-based requesting, only specimen request forms provided by histopathology should be used to request specimen testing. These forms should not be photocopied.
Any fresh specimens (not delivered in formalin) should be delivered directly to a member of histopathology staff to ensure processing is undertaken quickly with no degradation to specimen.
If you have any queries or should extra transport be required for any reason please contact the Trust transport department via switchboard.
All specimens should be transported in the relevant fixative or transport medium as indicated below in section 5. All specimen pots should be tightly sealed and transported using specimen bags, where appropriate. The request card should be placed in the pocket of the specimen bag, and the pot inside the sealed bag to ensure the safety of all staff.
Any specimens sent via Royal Mail should adhere to the packaging guidance available on the Royal Mail website. It is the responsibility of the sender to ensure that specimens are appropriately labelled, packaged and tracked.
TopSpecimen tracking
Many of our service users have systems in place to track specimens. If specimen acceptance criteria are applied at the time of tracked receipt, the specimen can be returned to the sender quickly should any discrepancy be identified.
Appropriate action in the event of a specimen acceptance failure involving fresh tissue (e.g. frozen section, gel sample) or an Urgent/HSC 205 sample is decided at the discretion of the reporting pathologist. The decision to accept and process pending confirmation may be taken.
If a specimen has been requested using HIVE, the sender can use HIVE to check whether the specimen has been received.
Top (Last reviewed August 2025)
 In this section
In this section