By Jo Adaway
Consultant Clinical Biochemist
March 2025
You’ve probably noticed that labs ask for a lot of information when you are requesting tests, and it may not be immediately obvious why some of this information is so important. One example of information we need is the time a sample was collected. This is needed because different analytes are stable for different amounts of time in whole blood once the sample is taken from the patient. Potassium, for instance, is only stable in blood samples for 10 hours at room temperature, because after this blood cells start to break down and release their intracellular potassium, giving a falsely raised result. If the date and time of collection given is more than 10 hours before the time the sample is received, our analysers will not measure potassium on the sample because of the risk of giving a falsely raised result.
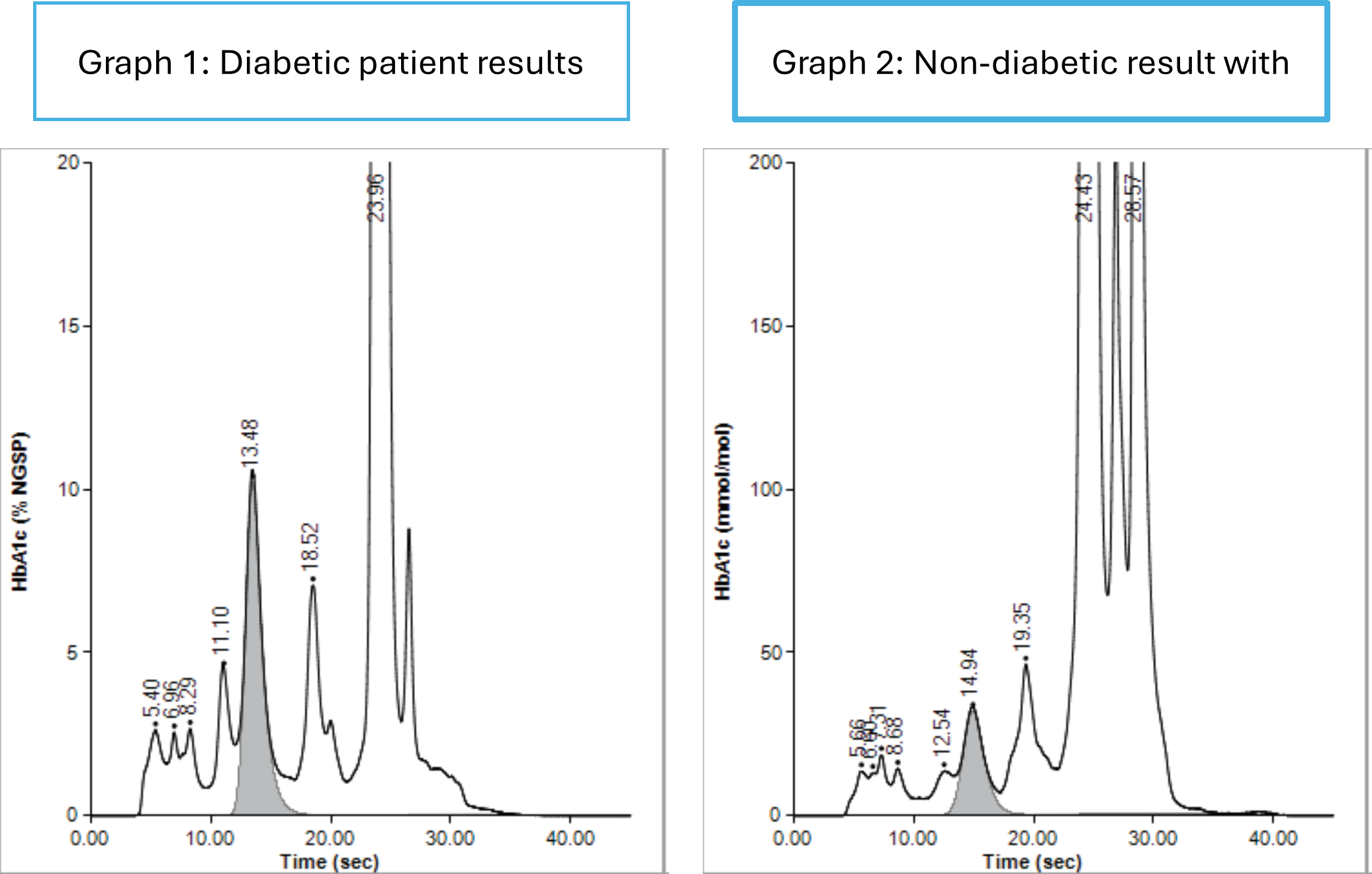
We also ask questions at sample collection to ensure we perform the correct test for the clinical situation, and to ensure we provide the correct clinical interpretation for the test. We recently introduced collection questions for HbA1c to ensure we know which samples are being taken to determine if a patient has diabetes, and which are being used to monitor patients known to have diabetes. This enables us to flag results consistent with non-diabetic hyperglycaemia (HbA1c 42-47 mmol/mol) to help you carry out the correct interventions for these patients. The other advantage of knowing which tests are being used to monitor patients with diabetes is that our HbA1c analysers can identify if there is an abnormal or variant haemoglobin present in the sample (figure 1). Most of these do not interfere analytically, but may indicate that the patients’ red blood cell turnover may be abnormal and the result cannot be used for the diagnosis of diabetes as the HbA1c cut-off for diabetes is based on a normal red blood cell lifespan. If a HbA1c is being used to monitor diabetes, we can still report the result in this case as the patient is acting as their own control, and their red blood cell turnover will remain constant for them.
Figure 1 HbA1c traces. Graph 1 shows a sample with a raised HbA1c and no abnormal haemoglobin present. Graph 2 shows a sample with a normal HbA1c but with a variant present. This will be reported if the test was requested to monitor a patient with diabetes, as the HbA1c is completely separated from the variant peak, but if the request was to diagnose diabetes, this result will not be reported as the HbA1c could be falsely low due to increased red blood cell turnover.
Thyroid function tests also have requesting questions in the ICE system. These were introduced to find out which tests are being requested on patients treated with thyroxine for primary hypothyroidism, as the TSH concentration is used to guide treatment in these patients, and the fT4 can be misleading as the concentration varies depending on when the sample was taken in relation to the thyroxine dose. The questions in the ICE system are to ensure that fT4 is analysed for patients that need it, such as those not on thyroxine, pregnant hypothyroid patients and those treated for thyroid malignancy or secondary hypothyroidism. Comments are added to many of our thyroid results, some automatically by our IT system and some by our Duty Biochemists, and the comment added is based on the information we are given by the person requesting the test. The same results can be interpreted in very different ways, depending on the clinical information we are given. It is crucial that the information given on the request is correct as the interpretative comment goes onto the patient record and can often be seen by the patient. If we take one set of results – TSH 4.65 mUl/L and fT4 12.9 pmol/L, the interpretation will be very different depending on the clinical information given in the answers to the ICE questions and in the clinical details field:
- Patient on thyroxine for primary hypothyroidism – Interpretation would be on TSH alone: Results suggest inadequate dose or treatment concordance. For patients on levothyroxine the biochemical goal of therapy is to normalise serum TSH. Refer to NG145 for management.
- Patient on thyroxine for secondary hypothyroidism: For patients on levothyroxine for central (secondary) hypothyroidism, the goal of therapy is to restore well-being and maintain FT4 within the upper half of the reference range.
- Patient on thyroxine and pregnant: In pregnancy, people taking levothyroxine for primary hypothyroidism should target TSH between 0.27 and 2.5 mU/L
- Patient on thyroxine, previous thyroid malignancy: For patients with previous thyroid malignancy, targets for TSH vary with the clinical context. Contact Endocrinology/Clinical Oncology team if further advice is required.
- Patient not known to have hypothyroidism: Slightly raised TSH, may be due to transient causes of elevated TSH including intercurrent illness. If clinical suspicion of thyroid disorder, suggest repeat in 3-6 months.
The interpretative comments that are added to Biochemistry results go into the patient record and may be seen by the patient. Erroneous interpretation of results due to incorrect details given at request could cause confusion and anxiety for a patient, if for instance the comment suggests the patient has secondary hypothyroidism or thyroid malignancy when this is not the case.
Accurate clinical information is incredibly important to ensure that we provide the correct interpretation for biochemical results, and that the correct information goes into the patient record. Incorrect information can lead to anxiety and confusion for patients who can view their records, and can mean that the correct action is not taken in response to results.
 In this section
In this section